The supply of oxygen (O2) is crucial for life and there are two ways O2 can be carried in blood: dissolved or combined with hemoglobin.
Dissolved O2 can only supply a fraction of what the human body needs. One mL blood holds only about 0.003 mL O2 at a partial pressure of oxygen (PO2) of 100 mmHg, and this can only be changed if we increase the PO2 (not easily done) or the solubility of O2 in blood (also not easy). And 0.003 mL O2/ mL blood is not enough.
To put it in perspective, a human with an O2 consumption of 250 mL and only a dissolved supply of O2 would need a cardiac output (blood pumped by the heart) of 83 L/min if the O2 extraction was perfect (hint: it is not). The heart normally pumps 5-6 L/min, and even top Olympic athletes don’t go much above 40 L/min. With the heart ejecting a maximum of 200 mL blood per beat (again, in athletes), that means we’d need more than 400 beats per minute to get to a cardiac output of 83. If we take into consideration that O2 extraction fraction is 25-30%, these figures increase to a cardiac output of 333 L/min and a heart rate of 1665 beats per minute, almost three times that of your average mouse heart rate.

Hemoglobin (Hb), fortunately, is a gamechanger.
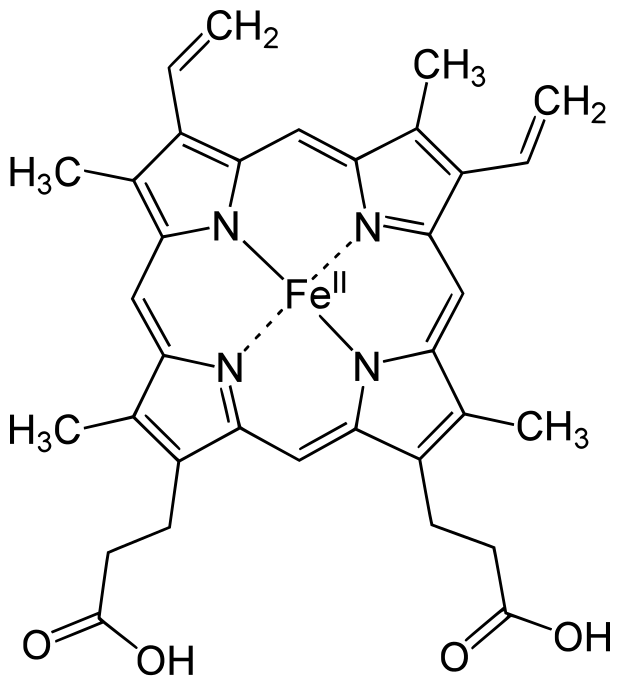
It is a molecule in red blood cells that has a central protein portion (globin), with four protoporphyrin (heme) groups attached, each with a ferrous (Fe2+) iron atom. This Fe2+ atom has a free binding side, which is where O2 binds. In effect, one Hb can bind four O2 molecules. And it does so reversibly. This means that O2 bound in the lungs can be easily released in the tissues.
The capacity of Hb to carry O2 is huge. It allows us to move away from the 83 L/min scenario above, to a much more reasonable required cardiac output. To illustrate how much of a gamechanger Hb truly is:
If a person has 15 g Hb per dL blood, and the O2 carrying capacity of Hb is 1.31 mL/g (normal conditions – the ideal capacity is 1.34 mL/g), it follows that this person’s Hb can carry:
15 g/100mL x 1.31 mL/g = 19.65 mL(O2)/100mL(Blood)
Add this to the dissolved O2 and take O2 exchange fraction into account:
(19.65 mL/100mL + 0.3 mL/100mL) * 0.25 extraction = 4.99 mL(O2)/100mL(Blood)
Calculate cardiac output:
250 mLO2/min / (4.99 mlO2/100mL) = 5012 mL/min = 5.01 L/min
This, of course, means that O2 transport in humans is heavily Hb dependent. The more Hb, the better the O2-carrying capacity. It is this principle that is at the core of blood doping and the use of illegal products like EPO to stimulate red blood cell production in competitive sports. Max physical performance depends on max O2 uptake, which is determined by cardiac output, O2 extraction (how well O2 enters the tissues) and Hb concentration. Of the three, Hb concentration is the only factor that can be artificially manipulated with relative ease to the increased performance of the athlete cheater.
But Hb contributes in other ways than simply by blunt concentration, and it does so by changing its affinity for O2.*
The affinity of Hb for O2 is simply the ease with which O2 is bound and released by Hb. Low affinity means that Hb binds less O2 for any level of PO2 (i.e. O2 is released easily, but not bound easily), and high affinity means that Hb binds more O2 for any level of PO2 (i.e. O2 is not released easily, but bound easily). This is usually described in terms of shifts on the oxyhemoglobin dissociation curve (below).

The relationship between PO2 and O2 bound to Hb is S-shaped, since the heme groups in Hb bind or release O2 one by one rather than independently of each other. This means that it doesn’t matter much for the actual O2 content of the blood if the PO2 is 70 mmHg or 100 mmHg – Hb is still quite saturated, thank you very much. PO2 in venous blood can fall to 40% under normal circumstances, and we only see a drop in Hb saturation to 75%.
There are mechanisms that can shift this curve, however, including: pH, partial pressure of CO2 (PCO2), 2,3-BPG (produced by red blood cells) and temperature. High acidity, high PCO2, high 2,3-BPG and high temperature lower the affinity (right-shift), and vice versa (left-shift). The shifting of this curve has some interesting physiological consequences.
As blood moves from the lungs into the tissues and gets more O2-poor (deoxygenised), PCO2 increases due to tissue metabolism. This causes a right-shift of the curve. PCO2 can also cause a further right-shift by reacting with water to form H+ and bicarbonate (HCO3-), thus lowering the pH in the blood. We can measure this acidity in venous blood (pH: 7.32 – 7.42, compared to arterial blood pH: 7.35 – 7.45). This together means that as the blood gets deoxygenised, Hb loses some of its affinity for O2, releases O2 more easily, and the O2 delivery can therefore be maintained until the blood returns to the lungs. There, CO2 is offloaded and pH normalised, returning the affinity to normal.
Of course, whilst Hb is essential, it is no guarantee. There are diseases caused by Hb malfunction or damage (sickle cell anaemia, for example), and at lower levels of O2, even Hb fails. For PO2 levels below 60 mmHg, there is a rapid decline in Hb saturation, and therefore also in O2 delivery to the tissues. We’re entering the realm of hypoxia. Down this road lies headaches, dizziness, increased pulmonary blood pressure, increased production of red blood cells, breathlessness, confusion, rapid heart rate and lowered blood pressure (except for in the lungs). This eventually leads to some pretty nasty consequences: cyanosis, right heart ventricle enlargement and failure, and death. The severity of the symptoms depends on how rapid and severe the O2 deprivation is.
Some of these symptoms, however, may be lessened by increasing Hb concentration. And one way to do this, is through iron. The Fe2+ component of Hb is a limiting factor in its production. The body has a store of iron to draw upon, called ferriting, but under long-term hypoxic conditions, such as travelling at altitude, the body will increase its uptake of iron from food, facillitating the generation of more Hb. We can also add iron intravenously. This can limit some of the body’s harmful responses to hypoxia, such as high pulmonary blood pressure, to almost nothing.
Adding iron to your diet is risky in the Marvel Universe. 
* O2 concentration in the blood can also be affected by PO2 and the gas exchange in the lungs. Neither are easily changed. PO2 is dependent on atmospheric pressure, and gas exchange is optimised in healthy individuals so that ventilation (V) matches blood perfusion in the lung (Q) perfectly – a V/Q ratio of 1.

Thanks for putting it so clearly. What are the effects of having an hemoglobin mutation/varient having low affinity for oxygen? Would the delivery to the tissue automatically compensate for lower oxygen saturation or could there be clinical maifestations?
LikeLike
That depends. Sometimes (0ften) there are no clinical manifestations with Hb mutations, and sometimes there are. The most well-known Hb mutant in humans is probably the sickle-cell variant, which causes amongst other things lowered oxygen affinity and anemia. Several other variants have also been linked to anemia, although symptoms may be due to the clinical instability of such variants rather than direct oxygen delivery issues. Heightened affinity is also not good, and sometimes compensated for by increased levels of red blood cell production (erythrocytosis).
LikeLike