Gases and physiology go hand in hand. We breathe oxygen and exhale carbon dioxide. Several molecules that we usually come across in gas form act as signal molecules, for example carbon monoxide and nitric oxide. But sometimes, things go wrong when gases meet physiology. In this blog post, I will talk about one such situation: decompression sickness, also called the bends.

What, exactly, is the bends? The bends happens when a person has been under pressure and then that pressure is removed quickly, causing the gases that are normally dissolved in the body fluids to form bubbles. A typical situation is where someone has been diving deep underwater and then resurface too quickly*.
What causes it? The first thing we need to know is which gases are problematic, namely inert gases. There are inert gases in the body. An inert gas is a gas that, under the given conditions, does nothing – i.e. it doesn’t undergo chemical reactions. The inert gases in the body mostly sits there and does not take part in metabolism. Oxygen is not an inert gas in the body – it contributes to several physiological processes including respiration. Nitrogen, however, is an inert gas in the body – it does not contribute. It is the main inert gas in the air, and the most common culprit of the bends.
Nitrogen and other inert gases are typically dissolved in the bodily fluids. This process requires pressure. Henry’s Law describes the relationship between pressure and a gas dissolved in liquid. This law states that when pressure on a liquid is decreased, the amount of gas dissolved in the liquid will decrease to the same extent, and when pressure is increased, the amount of gas dissolved will increase. This means that if the human body is put under high pressure (e.g. when diving), the inert gases will be dissolved in the bodily fluids. This is not a problem. The gases are inert, doing nothing, so we can usually handle the extra amount. The problem occurs when the pressure is reduced, and it is reduced fast. If a diver is moving slowly from the high-pressure underwater environment to the surface, the gases being released may escape bit by bit as the person breathes out, which is fine. But if it happens fast, the lungs may not be able to keep up, and that causes trouble. The inert gases become un-dissolved in places where they really should not be: we get bubbles trapped in the body.
Bubbles are bad news. They disrupt blood flow and can cause damage. Bubbles can form in (or be transported to) any part of the body (although some places such as large joints are more at risk). This means that we can get a great range of symptoms, depending on where the bubbles form. The worst outcome is death, which can happen if the bubbles for example interrupt spinal cord function. Less severe outcomes, although still severely unpleasant, are seizures, paralysis, dizziness, pain, visual disturbances, breathlessness, nausea, incontinence and more. In short, we do not want bubbles of inert gas (usually nitrogen) interfering with our organ function.
The deeper and longer the dive, the more dangerous it can be. We know that pressure increases as you descend. At 10 meters, the pressure has increased from 1 atm (sea level) to 2 atm, and the same level of pressure will therefore be needed for the diving suit to remain inflated. For reference, one atmosphere is the pressure that the air exerts at sea level, and the pressure tends to increase with 1 atm for each 10 m increase in depth. In other words, each 10 m below the surface adds to the body of water pressing down on the diver. The further down, the more weight, and this weight is in addition to the weight of the air (1 atm at sea level).
At 1 atm (sea level), the oxygen content is approximately 21%, and nitrogen content is approximately 78%. The oxygen pressure is therefore 0.21 * 1 atm =0.21 atm, and the nitrogen pressure is 0.78 * 1 atm = 0.78 atm. There are other pressure units that this can be measured in, such as mmHg or Torr (1 atm = 760 mmHg = 760 Torr) and kPa (1 atm = 101.325 kPa), but we will stick to atm for now.
If a diver is given normal air (with the percentage composition described above), at 10 meters the oxygen pressure will be 0.21 * 2 atm = 0.42 atm, and nitrogen pressure will be 0.78 * 2 atm = 1.56 atm. At this pressure, the blood will start to dissolve the nitrogen. This means that the fluids in the body will contain increasing amounts of nitrogen until an equilibrium is reached. How much nitrogen ends up where in the body depends on the tissue composition. Fat, for example, can dissolve a lot of nitrogen, and will take a bulk share.
Dissolving nitrogen is a slow process, as is releasing dissolved nitrogen. The longer the dive, the more nitrogen is dissolved, and the longer it takes to release it afterwards.
So why nitrogen? Why not oxygen, or carbon dioxide? As a rule of thumb, for the bends to happen, the diver has to experience the gas in question at a pressure of at least 2 atm. This excludes both carbon dioxide and oxygen. Even at depth, carbon dioxide pressure simply does not increase much above its normal level (about 40 mmHg, or around 0.05 atm), and oxygen is used up by the tissues so it does not rise as much either*. Unless the diver uses a gas mixture with a different inert gas (e.g. helium), nitrogen will be the villain of the piece.
There are advantages to using other gases. Helium, for example, is less soluble than nitrogen. This means it dissolves faster into the body fluids, but it is also removed faster, reducing the risk of developing the bends. For long dives, this is good, but for short ones (where nitrogen simply would not have time to dissolve much), it’s not so good. One may ask why use an inert gas at all, if they are so problematic, and the simple answer is that pure oxygen under pressure is toxic**.
What about diving animals? Plenty of animals have an aquatic mode of life, and the list includes a variety of species from the odd rodent, ungulate and marsupial to penguins, seals and whales. Many of these dive to incredible depth, and they ascend and descend quickly.

Diving depths of marine mammals, not including the deepest diving whale (Cuvier’s Beaked Whale, 2992 m) or birds (deepest diving is Emperor Penguin at 565 m, and deepest diving flying bird is Brünnich’s guillemot at 210 m). The personal record of this particular mammal is 3 m, which was a proud, yet unpleasant, moment. *Record by Soviet submarine K-278 in 1984, data for current submarines classified. Image not to scale: the submarine was 117 meters long, making it around 4 times the size of a blue whale.
At depth, the lungs of diving animals are almost entirely collapsed and blood flow to the lungs limited. Some diving animals even have collapsible rib cages that forces the air out when they dive. This means that no nitrogen can enter the blood during the dive. Many diving animals have quite small lungs, possibly because of this (and because large lungs work as airbags, making diving difficult). The diving animals do not store oxygen in their lungs for their dives, but rather in their blood, and they are very particular in how they use what little oxygen they have.
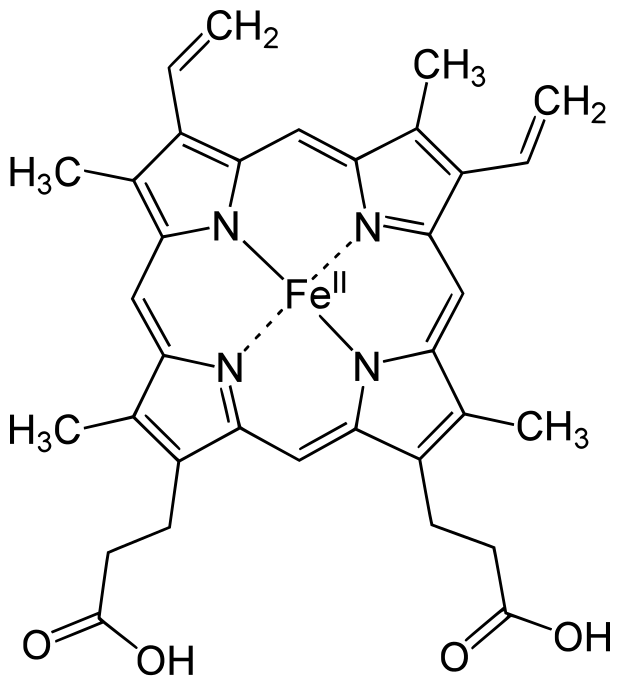
Oxygen storage. Diving animals usually have much more blood relative to their body size than non-diving animals, and the blood itself has a greater oxygen capacity (almost 40 ml oxygen per 100 ml blood, twice that of humans). The increased oxygen carrying capacity is due to a greater amount of red blood cells (which contain haemoglobin, the molecule that binds oxygen), and a much higher level of haemoglobin in the muscles (called myoglobin). The sperm whale, for example, has a myoglobin content almost 10 times that of humans, allowing them to store a vast amount of oxygen. Theoretically, the high level should cause the myoglobin to clump together, causing disease, but diving animals’ myoglobin is positively charged and stays nicely separated even when the muscles are packed with it.
Oxygen use. This impressive store of oxygen, however, is not enough. In addition, most diving animals have a lowered heart rate during dives, and blood flow to most of their internal organs is lowered (the exception being the brain). Even the heart gets less blood (but then again, the heart rate is lowered, so less blood is needed). Muscles also get reduced blood flow despite being needed to swim – instead, they rely on anaerobic (non-oxygen) metabolism after the myoglobin oxygen storage is depleted. Many diving animals also reduce muscle use. For example, Weddell and Elephant seals, bottlenose dolphins and blue whales have all been shown not to use their muscles when descending: sinking rather than swimming. And diving animals also reduce their metabolic rate, meaning that they use less energy. This is made easier by many diving animals being large, because oxygen consumption relative to body size is smaller the larger the body size. In other words: a mouse uses much more oxygen per gram of its body (1.65 litre oxygen per kilo per hour) than does an elephant (0.07 litre oxygen per kilo per hour).
In short: diving animals avoid the bends through minimizing the amount of nitrogen entering their blood when they dive***. To stay submerged, they are very good at storing oxygen in their blood (through higher blood volume and greater amounts of red blood cells) and muscles (through greater myoglobin levels), and use less oxygen (through shutting off blood flow to non-important organ systems, reducing their heart rate and metabolic rate, letting their muscles work anaerobically or not work at all).
*Interesting fact: The bends can also happen when ascending rapidly in for example an aircraft, with the danger arising as the pressure is quickly reduced to 0.5 atm. The underlying principles remain the same. A pressurised cabin will prevent this entirely (as with deep-diving submarines).
**Oxygen at pressures above 1 atm is toxic. When diving deeper than 60 meters, the pressure is so high that the gas mix needs to contain less oxygen than at sea level (hypoxic mixture) to avoid oxygen poisoning. There are multiple studies on oxygen toxicity, but the wikipedia article on the topic is quite extensive and accessible: https://en.wikipedia.org/wiki/Oxygen_toxicity
***This does not mean that they cannot get the bends. For example, stranded whales have shown signs of gas-bubble tissue damage (Gas-bubble lesions in stranded cetaceans: Nature 425, 575–576 (2003) https://www.nature.com/articles/425575a). It is possible that this has to do with the animals being stressed (and therefore either diving for too long or ascending or descending too quickly), or having too high blood flow (again due to stress or possibly also cold). While we do not know the exact reason why and how this happens, we do know that the use of sonar has been linked to whales getting the bends.






![By Anatomy_of_an_egg_unlabeled.svg: de:Benutzer:Horst Frank, SVG code cs:User:-xfi-, text removed by User:Kjoonlee derivative work: Vkkodali (Anatomy_of_an_egg_unlabeled.svg) [CC-BY-SA-3.0 (http://creativecommons.org/licenses/by-sa/3.0/) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons](https://upload.wikimedia.org/wikipedia/commons/f/fb/Anatomy_of_an_egg_labeled.jpg?w=680)